By: Graciella Davi & the NYCRA-NEWS Editorial team
Historically, there is substantial evidence of gross disregard and dismissive response on the part of the medical establishment in the way women have been diagnosed. Critics have speculated a vast array of reasons for this ‐ from professional carelessness and laziness to blatant sexism (and other forms of discrimination) to a lack of updated education in current research. But whatever the reasons may be, the lack of performance and attention in the hands of the medical diagnostician have resulted in tremendous danger to the patient. The most extreme cases of this underdiagnosing led to major health disorders and even death due to false negatives and missed conclusions from physicians and radiologists.
GILDA’S PLIGHT: “YOU’RE FINE…IT’S ALL IN YOUR HEAD”Our report starts with the legendary story of the late comedienne, Gilda Radner who died of ovarian cancer remission. In 1985, at a time when little information was available about this cancer, Ms. Radner started reporting pain in the upper legs and severe fatigue to her physicians'‐ whose diagnoses did not offer any satisfactory answers. Her recurrent issues worsened and she pursued other doctors for answers, some were said to have deemed her issues as 'mentally manifested'. By late 1986, her case had become so evident ‐ in the form of a grapefruit‐sized tumor from her abdomen, that she immediately underwent surgery and had a hysterectomy.
Gilda Radner's story carries many survivorship lessons, including the need to stay proactive about (your) cancer. Her journey also shows the importance of getting a second opinion, research for all diagnostic care options and staying vigilant about your continued health through early detection. But her story remains a landmark to all awareness crusaders who identify and expose this unfortunate trend that continues to plague women in health crisis to this day.
From a 2018 documentary called “Love, Gilda” (by Lisa D'Apolito), executive producer Meryl Goldsmith delivered a powerful and exclusive portrayal of the groundbreaking comic’s impact in our society as an entertainer and as one of the most powerful figures in cancer patient advocacy and survivorship. Ms. Goldsmith’s dedicated research on the life of Gilda Radner deeply explored her personal struggles including those pertaining to her health‐ leading to her untimely demise. "It's devastating to Gilda's family, friends, and fans, that she was not truly listened to when she complained of pains to doctors. Although she did end up with doctors who did the best they could to treat her, unfortunately she was delayed from getting the dire treatment she needed. Treatment was not as advanced as it is today, but early diagnosis was and remains crucial. We will never know if she would be alive today if doctors would have listened and looked carefully so they could have diagnosed it sooner."The world lost Gilda Radner in May 20, 1989, but many life‐saving lessons continue to resonate throughout the medical and patient communities from her story. She is an inspiration to advocates who push for a personalized treatment strategy. Ms. Goldsmith’s research and her film’s depiction of Gilda Radner’s treatment course stands as a major reference for any patient who may undergo similar struggles in getting proper treatment or accurate diagnoses.
THE FALSE NEGATIVE
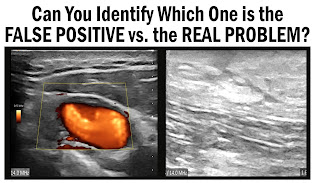
Over a decade after Gilda’s passing, Dr. Nancy Cappello (a startlingly similar case of professional inefficiency and neglect) was diagnosed with stage 3C breast cancer in 2004 from a mis‐read mammogram, concealed behind dense breast tissue. A false negative mammography scan unidentified a large 2.5 cm suspicious lesion, which was later found via ultrasound readings was confirmed to be stage 3c breast cancer. This same cancer had metastasized to 13 lymph nodes. This sparked Dr. Cappello to create the "Are You Dense?" Foundation‐ an international awareness crusade to better support dense breast diagnostics and initiatives pass legislation to enact laws requiring mammography centers to inform patients about their breast density and the associated cancer risks.
An excerpt from Nancy’s Story: “ I call it the best‐kept secret ‐ but it WAS known in the medical community. I have dense breast tissue – and women like me (2/3 of pre‐menopausal and 1/4 of post-menopausal) have less than a 48% chance of having breast cancer detected by a mammogram. In November 2003 I had my yearly mammogram and my "Happy Gram" report that I received stated that my mammogram was "NORMAL" and that there were "no significant findings." Six weeks later at my annual exam in January, my doctor felt a ridge in my right breast and sent me for another mammogram and an ultrasound… "Why didn't the mammogram find my cancer?" It was the first time that I was informed that I have dense breast tissue and its impact on missed, delayed and advanced stage cancer. What is dense tissue, I asked? Dense tissue appears white on a mammogram and cancer appears white – thus there is no contrast to detect the cancer (It is like looking for a polar bear in a snowstorm). I asked my physicians (now I had a TEAM of them) why wasn't I informed that I have dense breast tissue and that mammograms are limited in detecting cancer in women with dense breast tissue? The response was "it is not the standard protocol."
The disorder or the cause may vary, but sad endings to stories like these remain common in our patient community. We stand at a major point in history when medicine offers the highest advancements in technological innovations and treatment options- if not for HUMAN ERROR, or the mis-management of those entrusted to give professional care. So perhaps the most important lesson from Gilda Radner and Nancy Cappello 's story is to stay vigilant and "follow your gut". If something continues to feel wrong, trust your feelings. Never forget; doctors work for YOU. Never be railroaded to doubting your own feelings. There are MANY answers to cancer and they are all just a mouse click away.
By: Dr. Robert L. Bard
Nancy Cappello's "False Negative" led her late stage (type 3C) cancer, where the mammogram was not able to detect the cancer that was being concealed by her dense breast tissue. The lesson here is to upgrade the standard screening technology and expand to include supplemental scanning (such as the use of an ultrasound scan).
VIEWPOINTS:
It is apparent that science, technology and the medical community's desire to advance is truly upon us. Where current diagnostic resources are light years beyond where we were in the 80's and 90's, we are now able to find so many more answers to unique disorders once thought unfathomable. To instill better "detective work" on questionable unknowns (as part of medical due diligence) remains the clinical code of conduct of every physician and imaging specialist. Because of this, one can only hope to reduce or eliminate the level of negligence, false readings and (even) malpractice cases from underdiagnosed patients.
1) Gilda Radner/Illness: https://en.wikipedia.org/wiki/Gilda_Radner
2) Nancy's Story: https://www.areyoudense.org/stories/nancy/
4) Chronic fatigue syndrome: Gradually figuring out what’s wrong: https://www.health.harvard.edu/blog/chronicfatigue‐syndrome‐gradually‐figuring‐out‐whats‐wrong‐2019111418224
5) Video: Love Gilda- by Lisa D'Apolito (Magnolia Pictures/CNN Films): https://www.youtube.com/watch?v=1B44XRFotuo
Disclaimer & Copyright Notice: The materials provided on this website are copyrighted and the intellectual property of the publishers/producers (The NY Cancer Resource Alliance/IntermediaWorx inc., The AngioFoundation and Bard Diagnostic Research & Educational Programs). It is provided publicly strictly for informational purposes within non-commercial use and not for purposes of resale, distribution, public display or performance. Unless otherwise indicated on this web based page, sharing, re-posting, re-publishing of this work is strictly prohibited without due permission from the publishers. Also, certain content may be licensed from third-parties. The licenses for some of this Content may contain additional terms. When such Content licenses contain additional terms, we will make these terms available to you on those pages (which his incorporated herein by reference).The publishers/producers of this site and its contents such as videos, graphics, text, and other materials published are not intended to be a substitute for professional medical advice, diagnosis, or treatment. For any questions you may have regarding a medical condition, please always seek the advice of your physician or a qualified health provider. Do not postpone or disregard any professional medical advice over something you may have seen or read on this website. If you think you may have a medical emergency, call your doctor or 9-1-1 immediately. This website does not support, endorse or recommend any specific products, tests, physicians, procedures, treatment opinions or other information that may be mentioned on this site. Referencing any content or information seen or published in this website or shared by other visitors of this website is solely at your own risk. The publishers/producers of this Internet web site reserves the right, at its sole discretion, to modify, disable access to, or discontinue, temporarily or permanently, all or any part of this Internet web site or any information contained thereon without liability or notice to you.